Understanding Human Reproduction
Human reproduction is a complex and fascinating process that involves several key stages. Humans are sexually reproducing and viviparous, meaning the offspring develop inside the mother's body and are born live. Here’s a detailed look at the human reproductive process and the anatomy of the reproductive systems in both males and females.
The Reproductive Process in Humans
The human reproductive process includes several critical events:
- Gametogenesis: Formation of sperms in males and ova in females.
- Insemination: Transfer of sperms into the female genital tract.
- Fertilization: Fusion of male and female gametes to form a zygote.
- Blastocyst Formation and Implantation: Development of the blastocyst and its attachment to the uterine wall.
- Gestation: Embryonic development inside the uterus.
- Parturition: Delivery of the baby.
These events typically occur after puberty. Notably, sperm production in males continues into old age, while ovum formation in females ceases around the age of fifty.
The Male Reproductive System
The male reproductive system is located in the pelvic region and consists of several components:
Testes
- Location: Outside the abdominal cavity within the scrotum, which maintains a temperature 2–2.5°C lower than the body temperature, essential for spermatogenesis.
- Structure: Each adult testis is oval-shaped, approximately 4-5 cm in length and 2-3 cm in width, containing about 250 compartments called testicular lobules. Each lobule contains one to three highly coiled seminiferous tubules where sperms are produced.
- Cells: Seminiferous tubules are lined with male germ cells (spermatogonia) and Sertoli cells. Spermatogonia undergo meiotic divisions to form sperms, while Sertoli cells provide nutrition.
Leydig Cells
- Function: Located in the interstitial spaces outside the seminiferous tubules, these cells synthesize and secrete androgens (testicular hormones).
Accessory Ducts
- Components: Include the rete testis, vasa efferentia, epididymis, and vas deferens.
- Function: These ducts store and transport sperms. The seminiferous tubules open into the vasa efferentia through the rete testis, leading to the epididymis, which then connects to the vas deferens. The vas deferens ascends to the abdomen, loops over the urinary bladder, and joins with the seminal vesicle duct to form the ejaculatory duct, which opens into the urethra. The urethra extends through the penis to the external opening, facilitating sperm transport outside the body.
The Penis
- Structure: The penis is composed of specialized tissue responsible for erection, aiding in insemination. The enlarged end, known as the glans penis, is covered by a loose fold of skin called the foreskin.
Male Accessory Glands
- Components: Include paired seminal vesicles, a prostate, and paired bulbourethral glands.
- Function: These glands produce secretions that constitute seminal plasma, rich in fructose, calcium, and enzymes. Bulbourethral gland secretions also aid in lubrication.
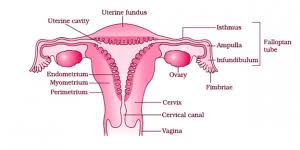
The Female Reproductive System
The female reproductive system is designed to support various reproductive processes, including ovulation, fertilization, pregnancy, and childbirth.
Ovaries
- Function: Primary female sex organs responsible for producing ova (eggs) and ovarian hormones.
- Location: Each side of the lower abdomen, connected to the pelvic wall and uterus by ligaments.
- Structure: Covered by a thin epithelium enclosing the ovarian stroma, divided into a peripheral cortex and inner medulla.
Oviducts (Fallopian Tubes)
- Function: Facilitate the transport of ova.
- Structure: Comprise infundibulum, ampulla, and isthmus regions, with finger-like projections (fimbriae) aiding ovum collection.
Uterus
- Structure: A single, pear-shaped organ supported by ligaments attached to the pelvic wall, opening into the vagina through a narrow cervix.
- Layers: Consists of three layers - perimetrium (outer layer), myometrium (smooth muscle), and endometrium (glandular lining undergoing cyclical changes).
Female External Genitalia
- Components: Include mons pubis, labia majora, labia minora, hymen, and clitoris.
- Function: These structures play roles in protection, sensation, and sexual arousal.
Mammary Glands
Structure of Mammary Glands
- Paired Structures: Mammary glands are paired and consist of glandular tissue and varying amounts of fat.
- Mammary Lobes: Each breast consists of 15-20 mammary lobes containing clusters of cells known as alveoli, responsible for secreting milk.
- Alveoli and Mammary Tubules: Milk produced by alveoli is stored in the cavities (lumens) of these structures, connected to mammary tubules that join to form mammary ducts.
Understanding Gametogenesis: The Process of Sperm and Ovum Production
Gametogenesis is a fundamental biological process where the primary sex organs, the testes in males and the ovaries in females, produce gametes - sperms and ova respectively. Here's a detailed look into the mechanisms and stages of gametogenesis.
Male Gametogenesis: Spermatogenesis
Overview
In males, spermatogenesis occurs in the testes and begins at puberty. This process involves the transformation of immature male germ cells, known as spermatogonia, into mature sperms.
Process
Multiplication of Spermatogonia:
- Spermatogonia are present on the inside wall of the seminiferous tubules.
- These cells multiply by mitotic division, increasing in number.
- Each spermatogonium is diploid, containing 46 chromosomes.
Formation of Primary Spermatocytes:
- Some spermatogonia periodically undergo meiosis to become primary spermatocytes.
Meiotic Division:
- The primary spermatocyte undergoes the first meiotic division, resulting in two haploid cells called secondary spermatocytes, each with 23 chromosomes.
- Secondary spermatocytes then undergo the second meiotic division, producing four haploid spermatids.
Transformation into Spermatozoa:
- Spermatids transform into spermatozoa (sperms) through a process called spermiogenesis.
- Post spermiogenesis, sperm heads embed into Sertoli cells and are released from the seminiferous tubules via spermiation.
Hormonal Regulation
Gonadotropin-Releasing Hormone (GnRH):
- Puberty triggers a significant increase in GnRH secretion from the hypothalamus.
- GnRH stimulates the anterior pituitary gland to secrete luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
Luteinizing Hormone (LH):
- LH acts on Leydig cells in the testes, stimulating androgen synthesis and secretion.
- Androgens promote spermatogenesis.
Follicle-Stimulating Hormone (FSH):
- FSH targets Sertoli cells, stimulating the secretion of factors that assist in spermiogenesis.
Understanding the Structure and Function of Sperm
Sperm, the male gamete, is a microscopic yet highly specialized cell essential for human reproduction. Let's delve into the detailed structure and function of sperm, as well as the process of sperm maturation and its role in fertilization.
Sperm Structure
A sperm cell consists of four main parts: the head, neck, middle piece, and tail. Each part plays a crucial role in the sperm's ability to fertilize an ovum.
 |
| SPERM |
Head:
- The sperm head contains an elongated haploid nucleus that carries genetic material.
- The anterior portion of the head is covered by a cap-like structure known as the acrosome, which is filled with enzymes that aid in penetrating the ovum during fertilization.
Neck:
- The neck connects the head to the middle piece and acts as a junction for structural support.
Middle Piece:
- The middle piece is packed with numerous mitochondria, which are the powerhouses of the cell. These mitochondria generate the energy required for the movement of the tail.
Tail:
- The tail, or flagellum, provides motility to the sperm, enabling it to swim through the female reproductive tract to reach and fertilize the ovum.
A plasma membrane envelops the entire sperm, maintaining its structural integrity and protecting its components.
Sperm Count and Fertility
During coitus, a human male typically ejaculates between 200 to 300 million sperms. For normal fertility, it is crucial that:
- At least 60% of the sperms have a normal shape and size.
- At least 40% of the sperms exhibit vigorous motility, which is essential for successful fertilization.
Sperm Maturation and Transport
After being produced in the seminiferous tubules of the testes, sperms are transported through a series of accessory ducts, including the epididymis, vas deferens, seminal vesicle, and prostate. These structures play key roles in sperm maturation and motility:
- Epididymis: Serves as a storage site where sperms mature and gain the ability to move.
- Vas Deferens: Transports mature sperms from the epididymis to the ejaculatory ducts.
- Seminal Vesicle and Prostate: Add secretions to the sperms, forming seminal plasma. This fluid provides nutrients and enhances the motility of sperms, forming semen.
The combined secretions of these accessory glands and the sperms constitute semen, the medium through which sperms are delivered during ejaculation.
Hormonal Regulation
The functions of the male sex accessory ducts and glands are regulated by androgens, the testicular hormones. These hormones ensure the proper development and functioning of the male reproductive system, facilitating spermatogenesis and the maturation of sperms.
Oogenesis: The Formation of Female Gametes
Oogenesis is the process of forming a mature female gamete, or ovum, and it differs significantly from spermatogenesis in males. This intricate process begins during embryonic development and continues through a woman's reproductive years. Let's explore the stages of oogenesis and its unique characteristics.
Initiation of Oogenesis
Oogenesis begins during the embryonic development stage when millions of gamete mother cells, known as oogonia, are formed within each fetal ovary. Unlike spermatogenesis, no new oogonia are formed after birth. Here's a breakdown of the key stages:
Primary Oocytes Formation:
- During fetal development, oogonia divide and enter prophase-I of the first meiotic division, becoming primary oocytes.
- These primary oocytes get temporarily arrested in this stage.
Primary Follicle Development:
- Each primary oocyte is surrounded by a layer of granulosa cells, forming a primary follicle (Figure 2.7).
- From birth to puberty, many primary follicles degenerate, leaving only 60,000-80,000 primary follicles in each ovary by puberty.
Follicular Development
As a female reaches puberty, the primary follicles undergo several changes:
Secondary Follicle Formation:
- Primary follicles develop additional layers of granulosa cells and a new theca, becoming secondary follicles.
- The theca is divided into an inner theca interna and an outer theca externa.
Tertiary Follicle Formation:
- Secondary follicles transform into tertiary follicles, characterized by a fluid-filled cavity called an antrum.
- At this stage, the primary oocyte inside the tertiary follicle grows and completes its first meiotic division.
Meiotic Division and Polar Body Formation
The completion of the first meiotic division results in:
Secondary Oocyte and Polar Body:
- The division is unequal, producing a large haploid secondary oocyte and a small first polar body.
- The secondary oocyte retains most of the nutrient-rich cytoplasm, which is crucial for its development.
Mature Follicle (Graafian Follicle):
- The tertiary follicle evolves into the mature Graafian follicle (Figure 2.7).
- The secondary oocyte develops a new membrane called the zona pellucida.
Ovulation
The final stage of oogenesis involves the release of the mature ovum:
- Rupture of Graafian Follicle:
- The Graafian follicle ruptures, releasing the secondary oocyte (ovum) from the ovary.
- This release process is known as ovulation.
Menstrual Cycle:
The menstrual cycle is a crucial aspect of female reproductive health, occurring in female primates such as monkeys, apes, and humans. This cycle starts at puberty with the onset of the first menstruation, known as menarche, and continues until menopause. Let's explore the stages and hormonal changes involved in the menstrual cycle.
Menstrual Cycle Phases
The menstrual cycle spans an average of 28-29 days, starting from one menstruation to the next. Here are the key phases:
Menstrual Phase:
- Duration: 3-5 days.
- Description: Menstrual flow occurs due to the breakdown of the endometrial lining and its blood vessels, resulting in bleeding through the vagina.
- Trigger: Occurs if the released ovum is not fertilized.
Follicular Phase:
- Description: Primary follicles in the ovary mature into a fully developed Graafian follicle, while the uterine endometrium regenerates and proliferates.
- Hormonal Influence: Increased secretion of gonadotropins (LH and FSH) stimulates follicular development and estrogen production.
- Peak: Both LH and FSH reach peak levels around the 14th day, leading to the LH surge that induces ovulation.
Ovulatory Phase:
- Description: The LH surge causes the Graafian follicle to rupture and release the ovum, a process known as ovulation.
Luteal Phase:
- Description: Post-ovulation, the remaining Graafian follicle transforms into the corpus luteum.
- Hormonal Influence: The corpus luteum secretes high levels of progesterone, essential for maintaining the endometrium in preparation for potential implantation of a fertilized ovum.
- Outcome: If fertilization does not occur, the corpus luteum degenerates, leading to the disintegration of the endometrium and the start of a new menstrual cycle.
Key Hormonal Changes
The menstrual cycle is regulated by a series of hormonal changes:
- Gonadotropins (LH and FSH): These hormones are secreted by the pituitary gland and play a crucial role in follicular development and ovulation.
- Estrogens: Produced by growing follicles, these hormones help regenerate and proliferate the endometrial lining.
- Progesterone: Secreted by the corpus luteum, this hormone is vital for maintaining the endometrium and supporting early pregnancy.
Menarche and Menopause
- Menarche: The onset of the first menstrual cycle at puberty.
- Menopause: The cessation of menstrual cycles, typically around the age of 50, marking the end of the reproductive phase.
Menstrual Cycle Indicators
Cyclic menstruation is a sign of normal reproductive health, extending from menarche to menopause. Regular cycles indicate the body's readiness for reproduction, while the absence of menstruation can suggest pregnancy or other health issues such as stress or poor health.
Fertilization and Implantation:
The Journey Begins: Insemination and Sperm Transport
During copulation (coitus), semen is released into the vagina through the penis in a process known as insemination. The motile sperms then embark on a rapid swim through the cervix, into the uterus, and finally reach the ampullary region of the fallopian tube. It is in this crucial region that fertilization takes place, provided both the ovum and sperms are present simultaneously.
The Miracle of Fertilization
Fertilization is the process where a sperm fuses with an ovum. This occurs in the ampullary region of the fallopian tube. The sperm must first penetrate the zona pellucida layer of the ovum, triggering changes in the ovum's membrane to prevent the entry of additional sperms, ensuring only one sperm fertilizes the ovum.
The acrosome, a cap-like structure on the sperm, releases enzymes that help the sperm penetrate the zona pellucida and the plasma membrane of the ovum, allowing the sperm to enter the cytoplasm of the ovum. This entry induces the completion of the secondary meiotic division of the oocyte, resulting in the formation of a second polar body and a haploid ovum (ootid).
Formation of the Zygote
Following the penetration, the haploid nucleus of the sperm fuses with the haploid nucleus of the ovum, forming a diploid zygote with 46 chromosomes. This zygote is the first cell of a new individual, and the sex of the baby is determined at this very stage.
Determining the Baby's Sex
The chromosomal pattern in humans plays a crucial role in sex determination. Females have XX chromosomes, while males have XY chromosomes. Therefore, all ova produced by females carry the X chromosome. Male sperms, however, carry either an X or a Y chromosome. Consequently, the fusion of the ovum with a sperm carrying an X chromosome results in an XX zygote, which will develop into a female, while fusion with a Y-carrying sperm results in an XY zygote, which will develop into a male.
This chromosomal determination is why it is scientifically accurate to state that the father's sperm determines the sex of the baby, not the mother’s ovum.
Understanding Early Embryonic Development: Cleavage, Blastocyst Formation, and Implantation
Cleavage: The Journey Begins
The journey of embryonic development begins right after fertilization when the zygote starts its mitotic division, a process known as cleavage. As the zygote travels through the isthmus of the oviduct towards the uterus, it undergoes a series of mitotic divisions forming 2, 4, 8, and 16 daughter cells, known as blastomeres. When the embryo reaches the stage of 8 to 16 blastomeres, it is referred to as a morula.
From Morula to Blastocyst
The morula continues to divide as it progresses towards the uterus, transforming into a blastocyst. This stage is crucial for the next steps of implantation and pregnancy. The blastocyst comprises an outer layer of cells called the trophoblast and an inner cell mass. The trophoblast will eventually play a key role in embedding the embryo into the uterine wall, while the inner cell mass will develop into the embryo itself.
Implantation: The Beginning of Pregnancy
Once the blastocyst reaches the uterus, the trophoblast layer attaches to the endometrium. This attachment triggers a rapid division of uterine cells, which then cover the blastocyst. The blastocyst becomes embedded in the endometrium, a process known as implantation. This event marks the onset of pregnancy.
Key Points of Embryonic Development
- Cleavage: The zygote undergoes mitotic divisions forming 2, 4, 8, and 16 cells (blastomeres) as it travels through the oviduct towards the uterus.
- Morula Stage: The embryo, now called a morula, contains 8 to 16 blastomeres.
- Blastocyst Formation: As the morula continues to divide, it forms a blastocyst with an outer trophoblast layer and an inner cell mass.
- Attachment and Differentiation: The trophoblast attaches to the endometrium, and the inner cell mass begins to differentiate into the embryo.
- Implantation: The blastocyst embeds into the endometrial lining, marking the start of pregnancy.
Pregnancy and Embryonic Development
Understanding the intricate processes of pregnancy and embryonic development is essential for appreciating how life begins and sustains itself. This guide breaks down these complex events into manageable and informative segments.
Implantation and Early Development
After the blastocyst embeds into the uterine lining during implantation, finger-like projections called chorionic villi emerge from the trophoblast. These villi are enveloped by uterine tissue and maternal blood, creating an interconnected structure known as the placenta. The placenta is crucial as it forms the interface between the developing embryo (foetus) and the maternal body.
Functions of the Placenta
- Nutrient and Oxygen Supply: The placenta facilitates the transfer of oxygen and essential nutrients from the mother to the embryo.
- Waste Removal: It also aids in removing carbon dioxide and waste products generated by the embryo.
- Connection to Embryo: An umbilical cord connects the placenta to the embryo, enabling the exchange of substances necessary for growth and development.
Placenta as an Endocrine Organ
The placenta functions not only as a physical bridge but also as an endocrine organ, producing several vital hormones:
- Human Chorionic Gonadotropin (hCG): Maintains the corpus luteum and supports pregnancy.
- Human Placental Lactogen (hPL): Modulates the metabolic state of the mother during pregnancy to facilitate energy supply to the fetus.
- Estrogens and Progestogens: Essential for maintaining the pregnancy and supporting fetal development.
- Relaxin: Produced by the ovary in the later stages of pregnancy, it helps in preparing the birth canal for delivery.
During pregnancy, the levels of other hormones such as cortisol, prolactin, and thyroxine also increase significantly, supporting various aspects of maternal and fetal health.
Embryonic Development Stages
Immediately after implantation, the inner cell mass (embryo) begins to differentiate into three primary germ layers:
- Ectoderm: Forms the outermost layer, giving rise to the nervous system, skin, and hair.
- Endoderm: Develops into the innermost layer, forming the lining of the digestive and respiratory systems.
- Mesoderm: Emerges between the ectoderm and endoderm, giving rise to muscles, bones, and the circulatory system.
These three germ layers are the foundation from which all adult tissues and organs develop. The inner cell mass includes stem cells with the potential to differentiate into any cell type, highlighting their crucial role in organogenesis.
Key Features of Embryonic Development During Pregnancy
Understanding the milestones of embryonic development is essential for expecting parents and those interested in human biology. Here is a detailed overview of the major features of embryonic development at various stages of pregnancy.
Duration of Pregnancy in Humans and Other Animals
- Humans: Pregnancy lasts approximately 9 months.
- Dogs: Pregnancy lasts about 2 months (58-68 days).
- Elephants: Pregnancy lasts around 22 months.
- Cats: Pregnancy lasts about 2 months (63-67 days).
Embryonic Development Stages
First Month:
- Heart Formation: By the end of the first month, the embryo’s heart is formed. The heartbeat can be detected with a stethoscope, marking the first sign of a growing fetus.
Second Month:
- Development of Limbs and Digits: By the end of the second month, the fetus develops limbs and digits, giving it a more recognizable human shape.
First Trimester (End of 12 Weeks):
- Major Organ Systems Formation: By the end of the first trimester, most major organ systems are formed. This includes the well-developed limbs and external genital organs.
- External Genital Organs: The external genital organs become well-defined.
Fifth Month:
- First Movements and Hair Growth: The fetus begins to show its first movements. Additionally, hair starts to appear on the head, which is a significant milestone in fetal development.
Second Trimester (End of 24 Weeks):
- Fine Hair and Eyelash Formation: The fetus's body becomes covered with fine hair, known as lanugo. Eyelids separate, and eyelashes are formed, indicating further development of facial features.
End of Nine Months:
- Full Development: By the end of the nine months, the fetus is fully developed and ready for delivery. All major organs and systems are mature and capable of functioning outside the womb.
First Month:
- Heart Formation: By the end of the first month, the embryo’s heart is formed. The heartbeat can be detected with a stethoscope, marking the first sign of a growing fetus.
Second Month:
- Development of Limbs and Digits: By the end of the second month, the fetus develops limbs and digits, giving it a more recognizable human shape.
First Trimester (End of 12 Weeks):
- Major Organ Systems Formation: By the end of the first trimester, most major organ systems are formed. This includes the well-developed limbs and external genital organs.
- External Genital Organs: The external genital organs become well-defined.
Fifth Month:
- First Movements and Hair Growth: The fetus begins to show its first movements. Additionally, hair starts to appear on the head, which is a significant milestone in fetal development.
Second Trimester (End of 24 Weeks):
- Fine Hair and Eyelash Formation: The fetus's body becomes covered with fine hair, known as lanugo. Eyelids separate, and eyelashes are formed, indicating further development of facial features.
End of Nine Months:
- Full Development: By the end of the nine months, the fetus is fully developed and ready for delivery. All major organs and systems are mature and capable of functioning outside the womb.
Parturition and Lactation:
As you prepare for the arrival of your little one, it's crucial to understand the natural processes of childbirth and breastfeeding. Here's a comprehensive overview of parturition (childbirth) and lactation (milk production) during pregnancy:








.png)
.png)

.png)

0 Comments